James Donaldson notes:
Welcome to the “next chapter” of my life… being a voice and an advocate for mental health awareness and suicide prevention, especially pertaining to our younger generation of students and student-athletes.
Getting men to speak up and reach out for help and assistance is one of my passions. Us men need to not suffer in silence or drown our sorrows in alcohol, hang out at bars and strip joints, or get involved with drug use.
Having gone through a recent bout of depression and suicidal thoughts myself, I realize now, that I can make a huge difference in the lives of so many by sharing my story, and by sharing various resources I come across as I work in this space. http://bit.ly/JamesMentalHealthArticle

Encouraging Your Young Adult to Seek Treatment
Even when adolescents or young adults are willing to consider treatment, it’s not uncommon for them to still feel hesitant or unsure. They may think that the problem “isn’t that bad” or that there’s no need for formal treatment. A child may think that help is needed for only the mental health part, like anxiety, but not substance use problems. In some cases, he or she may be reluctant to try treatment for fear that it will get in the way of school, work, sports or other activities. Stigma related to treatment may be a contributing factor to this resistance, too.
So how do you convince your son or daughter to try treatment? Prepare yourself before you sit down to have this important discussion. The following guidelines may help:
- Make an effort to see matters from your child’s point of view. How will treatment benefit your child? Will he feel healthier? Will she be more successful at school, work or sports? Will he get into the college of his dreams? What will your child see as the downside of treatment? Will he have trouble socializing without substances? Will she have to give up certain friends? Acknowledging both the positive and not-so-positive aspects of engaging in treatment can help the conversation go more smoothly.
- Determine what’s important to your child and frame the conversation. For example, some kids are reluctant to talk about substance use, but may be more comfortable talking about their mental health problem, such as depression or anxiety. If this is the case, talk about getting help for the area that they are willing to work on. Discuss with the treatment team you choose how to include other concerns.
- Do your homework and be ready with treatment options. Research programs to find ones that are a good fit for your child. If possible, it helps to offer options so that young people can make their own decision as opposed to being told what to do. For some kids, starting with a “consultation” with a counselor is less threatening than talking about long-term treatment.
- Use motivational “hooks.” Highlighting what your adolescent or young adult might gain related to treatment (e.g., better sleep, higher self-esteem, less stress) will likely be better received than talking about substances to give up. Some parents use incentives tied to something a child wants as a way to get them to engage in treatment. For instance, you could say something like, “If you complete eight outpatient sessions, we can discuss getting the video game you want.”
- Consider past attempts. If previous attempts to suggest treatment haven’t worked as planned, take time to consider why the discussion didn’t go well. What didn’t work? What would you change? Was the discussion too lengthy? Was it bad timing? What got in the way? Try to incorporate what you’ve learned to make this go more smoothly, including the timing of the conversation, a collaborative tone of voice, providing options, and incentives.
- Consider barriers to treatment. Does your insurance cover the cost of co-occurring treatment? Can you pick up costs that aren’t covered? Will transportation to and from treatment be a problem? Will your child be able to keep up with school? Address these matters before you talk to your child.
- Practice what you want to say. Once you have gathered the relevant information suggested above, it can be helpful to write down what you want to say. As you write, think about how your child might respond.
A Note About Required Consent for Treatment
If your child is a minor under the age of 18, you may assume that your consent is sufficient to get treatment started; however, this may not be the case. State laws vary considerably in terms of age of consent, in some instances being as low as 12 years of age. Additionally, who can consent may change depending upon whether the treatment program is for mental health or substance use and whether the facility is outpatient or inpatient. Often there is no guidance in situations where the parent and child disagree, leaving it up to the courts to figure it out.
If your child refuses to consent, asking other family members or friends to step in may help, especially if there is someone your child trusts and respects. Some parents look to educational or religious organizations to forcefully encourage young people into treatment, although research shows that outcomes are more likely to be positive if your child voluntarily agrees to treatment.
Alternatives to Treatment
If your child flatly refuses to seek treatment, there may be other healthy alternatives to consider in the meantime. Mindfulness meditation, for instance, is an effective way for many people to decrease their use of drugs and alcohol and has also been proven to help with depression, anxiety, and other mental health disorders.
Exercise is another useful strategy. It may be worthwhile to pay for a gym membership or yoga or dance classes. Is your child interested in music? Guitar or singing lessons may be a great diversion and an excellent way to increase confidence and self-esteem.
There are a number of ways kids can get help and support, even if they aren’t ready to make significant, long-term changes. An agreement to experiment with abstinence or to reduce their substance use by engaging in healthier activities can be considered a big win that often leads to greater changes.
Addressing Crisis Situations
Call 911 immediately if you’re concerned that your child is violent or may be suicidal or overdosing. Tell responders that your child is having a mental health emergency with as many details as possible so they can be prepared when they arrive. You can also call the National Suicide Hotline at 1-800-273-8255. The free hotline is available 24 hours every day.
- Some states offer mobile response services that respond 24 hours a day, seven days a week, providing help at your home to assess your child and help calm the situation. In addition, services include supportive counseling and referrals to community-based mental health, usually provided free of charge.
- You may consider driving your child to the nearest emergency room or crisis center, but only if you can do it safely. If possible, call and let the ER know when you leave, so they can be prepared when you arrive. If you don’t feel you can drive, ask for recommendations on what you should do next. Don’t transport a child against his or her will.
Non-Emergency Situations
If you think your child isn’t in immediate danger but is still in need of help, there may be several options to consider depending on available services in your state or community. The following suggestions may help you determine the best course of action:
- If your child has a therapist or treatment team (e.g. psychiatrist, therapist, nurse, etc.), they should be the first point of contact. People who know your child’s history are in a good position to help you figure out the next step.
- Call your local community mental health crisis center, which can be found using an internet search. Specific services vary widely depending on the state or county, but most offer specialized outpatient treatment for youth. Staff usually includes a team of mental health professionals, such as psychologists, psychiatrists, social workers, and nurses.
Regardless of whom you call, the first step is an evaluation or screening. Every effort will be made to understand your child’s needs and to consider various alternatives for treatment.
Quality Treatment and How to Get It
If you’re concerned your child has co-occurring substance use and mental health disorders, it will be helpful to consult a professional who is well versed in both mental health and substance use. This can include an evaluation with a qualified addictions professional. This evaluation can help to develop a preliminary diagnosis and a recommendation for the best treatment approach. Your child’s symptoms, age, gender, and culture, among other factors, will help determine his or her treatment plan.
Providers can be found using the Substance Abuse and Mental Health Services Administration(SAMHSA) or American Society of Addiction Medicine (ASAM) directories, Psychology Today or through your insurance provider, who may have an online portal to search specifically for addictions professionals. Evaluations usually take place in private practice or intensive outpatient setting, although some are done in hospital settings. Regardless of the setting, it’s important to talk to a person who is well-versed in both mental health and substance use to get a good read on what problems need to be addressed. For more information refer to Section Three, which covers differential diagnosis.
Depending on your child’s needs and how severe his or her symptoms are, there are several different levels of care. These include counseling, intensive outpatient programs (IOP), partial hospitalization programs (PHP) and rehab or residential care. Generally speaking, your child will be placed in what is considered to be the least restrictive level of care.
The most effective treatment for co-occurring disorders involves integrated care. This means that both mental health and substance use are treated at the same time by knowledgeable providers (for example, a psychiatrist, psychologist, case manager, medical team, etc.) who develop and implement an integrated treatment plan for both.
The treatment plan should include goals, objectives, treatment team members and their qualifications, evidence-based interventions including therapy and medications, and other services (such as vocational skills or academic supports) that will be offered.
Evidence-based interventions can include:
- Cognitive Behavioral Therapy (CBT)
- Trauma-Focused CBT (TF-CBT)
- Contingency Management
- Dialectical Behavioral Therapy (DBT)
- Motivational Interviewing (MI)
- Multisystemic Therapy (MST)
- Acceptance and Commitment Therapy (ACT)
Programs should also address physical health issues, whether offering on-site testing and counseling or referrals to other service providers. This can include issues like asthma, pain management, sleep disturbances, HIV, Hep C, and sexual health.
What Should You Look for in a Quality Treatment Programs?
- A comprehensive treatment plan to address mental health and substance use. Parents and/or the child (depending upon age) should be asked to agree to and sign off on the treatment plan. The treatment plan should be periodically reviewed and updated to reflect progress or modifications to the plan and approach.
- Programs that include a family component as part of the treatment plan to provide education, skill building, resources, and support. Often there is an opportunity to interact with other families to share what’s working and what can be improved.
- Programs that promote interactions with mentors, healthy activities and the recovery community. Often adolescents and young adults will need help engaging in activities like sports, volunteering and other organized social events; reconnecting with hobbies and interests that have gone by the wayside; and hanging out with healthier peers.
Many facilities advertise that they offer treatment for co-occurring disorders, but it’s important to do your homework and find out exactly what they mean by that. For instance, some providers won’t work on mental health issues until a person is totally abstinent from substance use. Others might say they treat co-occurring disorders, but what they really mean is that there’s a nurse on hand to dispense psychiatric medications or a psychiatrist who will write a prescription based upon the diagnosis your child was given prior to admission to the program.
Medications selected must take into account both substance use and mental health, as there are some medications that might not be recommended for people who struggle with substance use. For example, many practitioners won’t prescribe Adderall for ADHD or Xanax for anxiety due to their misuse potential.
Programs may offer yoga, meditation classes, art therapy, and other activities as supplements to treatment. Some programs may offer 12-step/mutual aid groups like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) or SMART Recovery on premises, or require that your child attend on days when he or she isn’t in programming at the facility. Other supports that may help include National Alliance on Mental Illness (NAMI)’s OK2Talk Program or the Depression and Bipolar Support Alliance (DBSA) support group.
Quality programs will develop a comprehensive discharge or continuing care plan, including referrals for a step down to a lower level of care (e.g. a PHP to IOP, or IOP to individual counseling and a psychiatrist). One critical component of continuing care is a relapse prevention plan that identifies high-risk situations or circumstances, early warning signs and symptoms, and flags or problems related to medications, providers, relationships, daily structure, transportation or finances. In addition, it may help to identify an “accountability partner” to help keep your child on track with healthy living and to discuss what the next steps will be should a relapse occur.
The Family Role in Supporting Your Child
The family role in supporting a child with co-occurring disorders is critical. This includes everything from recognizing that there is a problem, to motivating a child to get help, to navigating the treatment system to find the best fit for your child and helping him or her sustain gains in recovery. It can be a significant emotional, time and financial commitment, but research shows that family involvement improves outcomes. Families can also help ensure diagnosis is accurate.
In addition to the mechanics of getting treatment and providing information to the treatment team, you can also help in other ways:
Encourage Treatment Participation
Encourage your child to keep appointments and participate in all aspects of his or her treatment plan. This may include individual, group and family therapy, medications and job and life skill-building. If a case manager is working with your child, stay on the same page and provide input on progress made, as well as setbacks. Keeping a calendar of appointments and ensuring transportation is available if needed may be necessary.
Some parents use positive reinforcement to improve the chances that their child will stick with a treatment plan. Hearing that their parent is proud of them or receiving a letter from home while in residential treatment to keep them motivated can be very meaningful to young people. As a parent, you can also offer incentives for participating in treatment, as mentioned previously in Section Ten.
Provide Emotional Support and Encouragement
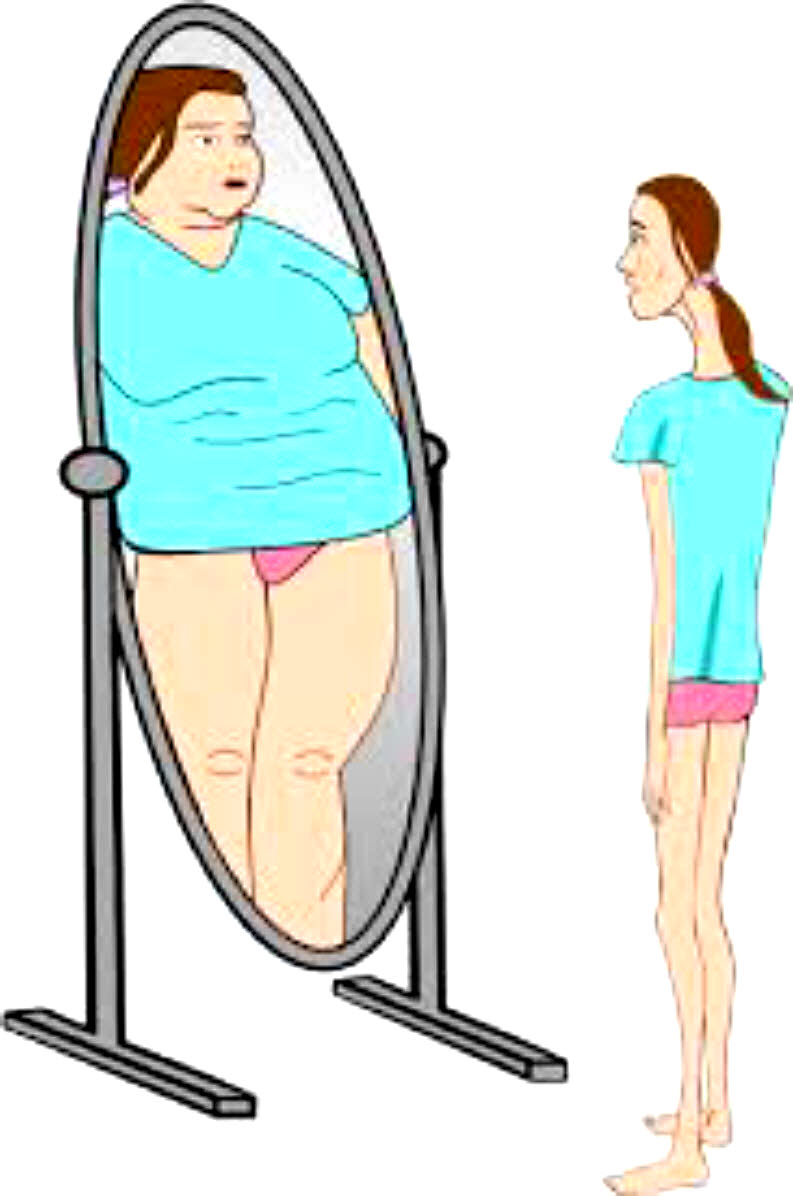
Often adolescents and young adults so desperately want to be “normal.” They don’t want to have to deal with treatment. They don’t want to take any medication. They are hyper-aware of stigma and may minimize one or both disorders as a result. Listening to concerns and being empathetic can go a long way toward helping them stay the course, in addition to simply letting your child know that you care.
Some adolescents and young adults have been to multiple treatment programs and may feel demoralized or that “nothing works.” You too may feel hopeless if your child needs treatment yet again. It can help both of you to reflect on any aspect of previous treatment that was useful (such as learning about his mental health challenges, finding a therapist that she liked, feeling better for even a short period of time, learning a new coping skill, meeting someone in treatment that he could relate to, etc.). It helps if you think about every treatment episode as an opportunity to build upon what was already learned.
Participate in Family Education
Many programs offer what is referred to as a psychoeducational group for families. These groups are provided so that families can learn more about mental health symptoms, signs of substance use, treatment options, medications, and relapse warning signs. It’s also a place where families can process what has happened since the last session and get advice as to how to respond more effectively if warranted.
A family weekend or four-day educational program is often offered in residential treatment settings. There are also designated times for visits and, in some cases, time off campus.
Attend Individual and Family Counseling
Participate in individual counseling and family counseling if offered, both with and without your child. These sessions can help you address concerns, improve family interactions and problem solve with the support of a counselor in a safe environment. Skilled therapists can help you and your loved ones learn how to relate to each other and respond effectively to build a stronger family.
Assist With Medication Management
In addition to providing input to doctors when prescribing medications to your child, you may need to fill prescriptions and give your child the medication, depending on his or her age. It can help to keep a notebook of the name of the medicine, the prescribed dosage, and what you notice with respect to side effects and symptom reduction. If multiple medications are needed, it can help to get a weekly pillbox from the pharmacy to organize pills rather than counting them out each day.
It isn’t uncommon for young people to be dissatisfied with their medications at first. This may mean that the medication they are taking has side effects they don’t like. It can also mean that the substances they were using did a better job of addressing their anxiety, boredom or other reasons for use. In either case, it can be helpful to discuss this with the treatment team to make adjustments if necessary. Often visits with psychiatrists are very brief — sometimes just 15 minutes — so being prepared to discuss how the medication is working is critical and can make the most of the session.
Encourage Abstinence
Alcohol and other drugs can worsen mental health symptoms and interact negatively with medications. Keep all substances out of your home, including household products that can be used as a substitute for alcohol (like hand sanitizers or vanilla extract), as well as products that can be sniffed or huffed (like keyboard dust cleaners). If you do keep alcohol or marijuana in the home for your personal use, keep it secured along with any medications that can be misused.
Help Establish Structure and Meaning
Co-occurring disorders can disrupt your child’s sense of purpose, throwing daily structure into a tailspin as substance use and mental health problems dominate your child’s life. Getting back to meaningful activities is one of the cornerstones of recovery and can help motivate your child to manage their mental health and provide reasons to stay sober. Asking about and encouraging involvement in school, work, volunteer activities, hobbies, sports, and other interesting activities is important.
Hopefully, the treatment team will guide you and your child in creating a purposeful, structured day, but if not, try to put a plan together with your child. A weekly planner can be helpful in terms of establishing a schedule for when to wake up, do chores, attend school or work, participate in recreational activities, attend counseling, etc. This is not to suggest that every minute of every day must be scripted, but it can help to set expectations and to identify gaps in your child’s schedule that can be filled with meaningful activities.
Promote Healthy Social Supports
Support groups can be a great way for your child to meet other people who understand what he or she is going through. Groups are also a potential source of resources and referrals, along with social supports for engaging in activities that promote well-being. Encourage attendance at meetings for substance use such as 12-step (e.g., AA or NA) and SMART Recovery. You can search for mental health peer support groups at association websites (e.g. Anxiety and Depression Association of America (ADAA), Depression and Bipolar Support Alliance (DBSA) or National Eating Disorder Association (NEDA). Dual Recovery Anonymous is a 12-step meeting specifically for people with co-occurring disorders. Many of these organizations have meetings that can be attended online or in person and have other useful content on their websites.
Your child may welcome your participation at a meeting or prefer to go alone or with a friend. Take your child’s lead on this issue, especially if he or she would prefer to attend without you being there. Your child may welcome the opportunity to share with the other members but be reluctant to say anything in front of you. Also, every meeting is different so if your child doesn’t care for one, encourage trying a different one.
One note of caution: Some participants at 12-step meetings believe that medications are a crutch and unnecessary for “true recovery.” This is not the official position of these organizations, with the exception of Narcotics Anonymous. NA has taken a position stating that anyone on medication-assisted treatment (MAT) for opioid use disorder is not abstinent. Despite overwhelming evidence that MAT can save lives, some NA meetings will limit the participation of anyone on MAT. If your child is on MAT, he or she may be better served by a different support group.
You can also help adolescents and young adults find and engage in sober recreational activities. Aside from support groups, recovery centers host outings (such as flag football, 5K runs, coffee houses, movies, game night, cooking classes, picnics, etc.) that may be of interest to your child. Many kids think they will never have fun again if they aren’t using substances, so helping them learn how to do this is an important part of recovery.
Join Family Support Groups
Support groups for families geared toward a loved one’s substance use include Al-Anon, Nar-Anon, Families Anonymous and SMART Recovery for Friends and Family. In addition, most of the mental health associations mentioned earlier provide supports to families as well. AA and Al-Anon as well as NA and Nar-Anon often host meetings at the same time and location. If the opportunity presents itself, it’s nice to attend and compare notes afterward over a cup of coffee or ice cream.
Foster Coping Skills
Help your child learn to address stress in a healthy way by developing coping skills. Stressors can be major, such as an unexpected loss, moving, attending a new school or starting a new job, or they can be minor, such as everyday annoyances or worries. Coping skills can help your child deal with these issues and with mental health symptoms related to depression, anxiety, sleep problems and hallucinations, as well as cravings to use substances.
Help your child process stressful experiences by being there as a sounding board to listen. It can help to ask questions like “What do you think you should do under the circumstances?” or “How do you think you want to handle this situation?” rather than jumping in with answers. While it may be tempting to solve problems for your child, it can undermine self-esteem and confidence. Reminding your child of coping strategies for managing stress can also be helpful, like taking deep breaths or learning to meditate. Your child’s treatment team should be able to provide advice about how to support your child in developing healthy coping skills.
Engage in Self-Care
Helping someone with co-occurring disorders is like being in a marathon than a sprint, so self-care is critical. Remember that if you fall apart, you won’t be able to help your child. Coping with your own stress without using substances, eating nutritious meals, exercising, taking medications as prescribed, getting regular sleep, attending support group meetings, etc., can help you feel better while modeling a healthy lifestyle for your child. Engaging in mindfulness practices (like yoga, breathing exercises, meditation, Tai Chi, or guided visualizations) can also be useful and can be done with your child or as a family.
Know the Signs of Relapse
It isn’t unusual for relapses to happen, despite quality treatment and your child and family’s best efforts. Knowing your child’s “vital signs” for both mental health and substance use disorders is important to head off a relapse as well as to address one should it occur.
The symptoms of relapse are often different for mental health and substance use so it may take some careful thought to identify what to look for. The treatment team and your child can be helpful in figuring out what the early warning signs are and what to do if you spot them. Having a relapse prevention plan in place can help shorten its duration, getting your child back on track to well-being.
Hope that things can be better is a powerful motivator that can strengthen a person’s desire and determination to attend to their health and well-being. You and other family members can play a critical role in helping your son or daughter feel hopeful, recognize that change is possible and that he or she can lead a wonderful, fulfilling life.
Resources for Co-occurring Disorders
It can be a huge help to educate yourself about substance use and mental health disorders. In addition to the Child Mind Institute (childmind.org) and Center on Addiction – Partnership for Drug-Free Kids (drugfree.org), there are many resources available. If your child is already engaged in formal treatment, consider asking your child’s treatment team for resources, too.
The National Institute of Mental Health (NIMH) offers information on disorders as well as clinical trials.
National Institute of Drug Abuse (NIDA) offers research on the state of the science in the occurrence of substance use disorders with mental illness and physical health conditions.
National Alliance for Mental Health (NAMI) offers a free, 12-week course in local communities called Family-to-Family for caregivers living with a loved one with mental health disorders.
Substance Abuse and Mental Health Services Administration (SAMHSA) offers free e-booklets and guides to download on various co-occurring disorders. They also offer a treatment locator service. It’s helpful to watch their short video to learn how to use their search capabilities.
Mental Health First Aid offers an 8-hour course to help participants recognize when a person is having a mental health or substance use challenge and how to help.
Crisis Text Line connects people with Crisis Counselors trained to bring texters from a hot moment to a cool calm through active listening and collaborative problem-solving.
Associations and alliances for mental health disorders may have useful resources to consider:
- Anxiety and Depression Association of America (ADAA)
- International OCD Foundation (IOCDF)
- National Eating Disorders Association (NEDA)
- Depression and Bipolar Support Alliance (DBSA)
- International Bipolar Foundation (IBPF)
- Schizophrenia and Related Disorders Alliance of America (SARDAA)
- National Alliance of Mental Illness (NAMI)
- Children and Adults with Attention-Deficit/Hyperactivity Disorder (CHADD)
- National Education Alliance for Borderline Personality Disorder (NEABPD)
The American Academy of Child and Adolescent Psychiatry (AACAP) offers a resource center with information on mental health disorders as well as substance use, bullying, suicides, trauma, etc.
The Brain & Behavior Research Foundation engages in cutting-edge research to find cures for mental illnesses. They also offer the Healthy Minds Public Television Series with Dr. Jeffrey Borenstein and webinars that are informative for public viewing.
MindTools.io rates platforms and apps for teens, adolescents, and adults related to mindfulness, stress management, insomnia, substance use, mental health, and counseling. Some of the apps are free while others have a nominal fee.