Welcome to the “next chapter” of my life… being a voice and an advocate for mental health awareness and suicide prevention, especially pertaining to our younger generation of students and student-athletes.
Getting men to speak up and reach out for help and assistance is one of my passions. Us men need to not suffer in silence or drown our sorrows in alcohol, hang out at bars and strip joints, or get involved with drug use.
Having gone through a recent bout of depression and suicidal thoughts myself, I realize now, that I can make a huge difference in the lives of so many by sharing my story, and by sharing various resources I come across as I work in this space. http://bit.ly/JamesMentalHealthArticle

ON A seemingly ordinary Thursday morning last May, respected Brisbane gastroenterologist Andrew Bryant went to work but never came home.
Shortly after arriving at his practice, the 54-year-old ended his life. He didn’t write a note, leaving his wife Susan and their four children to wonder what had gone so horribly wrong.
But the reality is that Dr. Bryant’s story is tragically common in Australia, with staggering rates of suicide in a vocation that’s devoted to health and wellbeing.
“I’ve learned that the medical profession is one of the worst industries statistically in terms of mental health outcomes,” Dr. Bryant’s son John, 26, told news.com.au
“Considering it’s a caring profession, it seems that far too many don’t care for themselves, which is surprising and alarming.”

Dr. Andrew Bryant took his life in May last year, part of a serious problem in the medical profession.
Data shows that medical professionals are more likely to die by suicide than the general population — female doctors 2.2 times more, male doctors 1.4 times.
Young doctors at significant risk, with 20 per cent of trainees experiencing suicidal thoughts.
A cluster of suicides among doctors over the past two years sent shockwaves through the profession and prompted an urgent response from the Australian Medical Association.
Reliable, recent figures are difficult to come by but the most indicative data shows that there were 369 suicides by health professionals between 2001 and 2012.
Today, a senior doctor who has lost three colleagues, published a powerful piece in the Medical Journal of Australia demanding widespread systemic change.
“In recent Australian surveys, one in five students reported suicidal ideation in the preceding 12 months, while 50 percent of junior doctors experienced moderate to high levels of distress,” Ann McCormack, an endocrinology specialist at St Vincent’s Hospital Sydney, wrote.
“What seems clear to me is that inherent traits in the individuals who choose a career in medicine, and often create excellent doctors, also set them up for high rates of distress.”
What’s happening to put our doctors in such precarious positions and what’s being done?
OUT OF THE BLUE
John’s beloved father, who exemplified the image of a community-minded family man, was the last person he expected to be at risk of suicide.
“My dad was a very energetic person and a lot of fun to be around,” the Brisbane paralegal recalled.
“He was quite generous with his time and involved in lots of different things, volunteering quite often. He was a good person. He was happy.
“As well as a gastroenterologist, he was an Air Force reservist. He loved to cycle on the weekends as a hobby and go sailing. He kept very busy.”
Throughout October and November, news.com.au has been highlighting the issue of men’s mental health with the campaign The Silent Killer: Let’s Make Some Noise in support of Gotcha4Life and Movember.
Gotcha4Life is dedicated to an in-school program helping educate young men about resilience and the importance of friendships and runs a scholarship program with Lifeline to train more males counselors.

John Bryant, pictured with his late father Andrew, said his dad was the last person to be at risk of suicide.
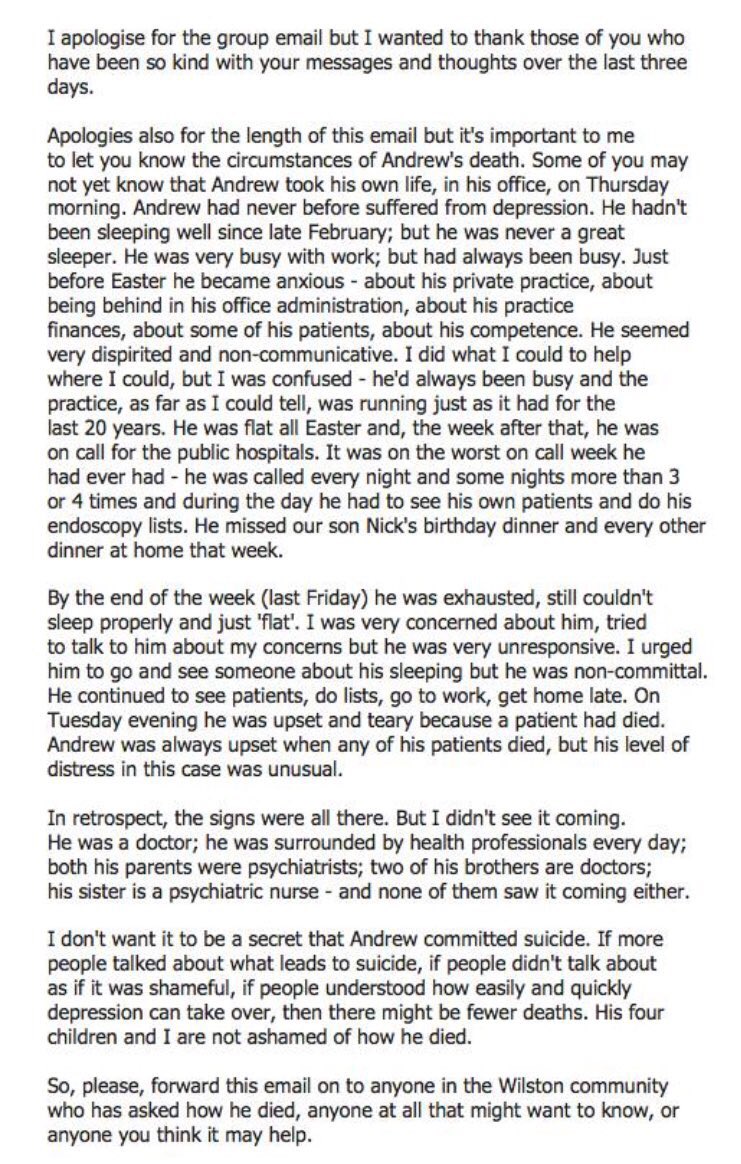
In the days following his death, Andrew’s grief-stricken wife Susan wrote a heartfelt email to her law firm colleagues to explain what had happened.
“I don’t want it to be a secret that Andrew committed suicide,” she said, encouraging recipients to share her words.
They did and the message quickly went viral on social media, adding to calls for more resources dedicated to reversing suicide rates among medical professionals.
“He hadn’t been sleeping well since late February, but he was never a great sleeper,” she said. “He was very busy with work, but he had always been busy. In retrospect, the signs were all there. But I didn’t see it coming.
“He was a doctor; he was surrounded by health professionals every day; both his parents were psychiatrists, two of his brothers are doctors, his sister is a psychiatric nurse — and none of them saw it coming either,”
John said his dad seemed a bit flat in the weeks before he died. Work was busy and he was more stressed than normal, but there was nothing significant to raise a red flag.
“In retrospect, there were signs that he was struggling but at the time it wasn’t enough to make us concerned. We thought he seemed a bit flat but not that he was at risk of suicide.”
Young trainee Sydney doctor Chloe Abbott took her life in January 2017, just months after cracks began to appear and her concerned family begged her to quit medicine.
Like so many others beginning their careers, she was juggling a 60-hour work week at a hospital with a 30-hour study load on top. It left no downtime to see her loved ones.

Chloe Abbott was lost in January 2017 to suicide due to the pressure of being a junior doctor. Source: Supplied
That’s not an anomaly. Data shows doctors aged 30 and under work the longest hours of any age group and industry in Australia.
That cohort also scores highest on the three measures of burnout risk in medicine — emotional exhaustion, high cynicism, and low professional efficacy.
Her colleagues thought she “had it all”, her mother Leonie said, and Chloe’s death “rocked them to their core and it shattered their beliefs”.
“They would be thinking if Chloe couldn’t do it, how can I do it?” Leonie said. “If Chloe couldn’t manage this life as a doctor, how on earth can I do it? Then they would look at themselves as far less resilient and capable than Chloe.”

Leonie Eagles with daughters Jessica and Micaela Abbott, who has taken on advocacy for mental health in medicine since the death of Chloe.
Her family has become lobbyists for a transformation of the “toxic” culture of medicine, which saw them receive a Pride of Australia medal for their work.
Dr. McCormack said she felt compelled to write about the still-taboo issue of doctors who suicide after a spate of personal experiences.
“Over a matter of months, two female junior doctors committed suicide at our hospital, and more recently, suicide entered my inner circle with the death of one my close male colleagues,” she said.
“Such stories are not unusual in our profession.”
OUR UNWELL DOCTORS
Dr. Bryant had never shown any signs of depression, anxiety or any other mental illnesses.
But around Easter last year, he seemed to be increasingly anxious about work. He was behind on administrative tasks, he began to doubt his abilities and his spirit appeared crushed.
“I did what I could to help where I could, but I was confused,” Susan said.
“He’d always been busy and the practice, as far as I could tell, was running just as it had for the last 20 years.”
A week later, he was on call for Brisbane’s public hospitals in what turned out to be “one of the worst on-call weeks he had ever had”, she said.

Dr. Andrew Bryant with his daughter Charlotte and wife Susan.

John Bryant has turned his attention to fundraising and raising awareness of mental health.
By the end of it, he was exhausted but still unable to sleep. The following Tuesday, he was distraught after the death of a patient.
“Andrew was always upset when any of his patients died, but his level of distress, in this case, was unusual,” Susan said.
Almost two years on, she has come face-to-face with the enormous internal and external expectations faced by doctors, and the alarming consequences it can lead to.
Before she died, Chloe wrote about the pressures she and her colleagues were feeling and implored the industry to change from within.
“As competition for places has intensified, academic research experience has become an increasingly significant point of difference for trainees, but this is yet to be reflected in many pathways currently available in Australia,” she wrote.
“Instead, trainees are burdened with meeting their clinical training requirements while simultaneously attempting to pursue academic research, often leaving them in difficult financial circumstances — the remuneration of these endeavors is significantly less than a full-time medical trainee income.”

Doctors are more likely to die by suicide than the general population, with women and trainee doctors at most risk.
Perfectionism is rife among doctors, Dr. McCormack wrote, which can contribute to success as well as a mental health downfall.
“Among the medical workforce, work-life balance is poorly practiced and modeled,” Dr. McCormack wrote.
“In fact, there is a subtle undertone rampant within the medical fraternity, in which late-night emails, missing a child’s school concert, publishing multiple articles a year, and not taking annual leave to become unvoiced indicators of a truly committed doctor.”
In addition to extraordinary pressure, numerous reviews and investigations have revealed a disturbing underbelly in medicine.
A 2016 survey in Victoria found 25 percent of health staff had experienced workplace bullying, while a similar probe in 2014 found 40 percent of nurses had been harassed in the previous 12 months.
In 2015, the Royal Australasian College of Surgeons found that 49 percent of respondents had been subjected to discrimination, bullying, harassment or sexual harassment.
And last year the Australasian College for Emergency Medicine released the results of a member survey that found 34 percent of respondents had experienced bullying, 21.7 percent discrimination, 16.1 percent harassment, and 6.2 percent sexual harassment.

Chloe Abbott’s mother Leonie Eagles has become an advocate for the issue of doctors who suicide.
Johanna Westbrook from the Australian Institute of Health Innovation at Macquarie University said the alarming trends posed a risk to both doctor and patient safety.
A Senate Inquiry conducted in 2016 into the medical complaints process in Australia recommended that governments, hospitals, colleges, and universities commit to eliminating bullying and harassment.
But Professor Westbrook said it “provided little direction as to how this should occur”.
Adding to the problem is a finding by Beyond Blue that 58 percent of doctors feel embarrassed when seeking treatment for mental health issues.
Abbott family win Pride of Australia award for mental health campaigning

A serious stigma is prevalent in medicine, particularly when it comes to conditions like depression and anxiety. According to Beyond Blue, 47 percent of doctors admitted they were less likely to employ someone who has a history of mental illness.
And 44 percent of doctors felt depression or anxiety were signs of weakness.
“If doctors do not deal with the mental health issues they are experiencing, it can affect their ability to deliver the best care,” the organization’s boss Kate Carnell said.
TRAINEE DOCTOR CRISIS
Following the spate of deaths in recent years, Australian Medical Students Association president Robert Thomas said greater support is needed.
“Students put in a lot of effort and a lot of emotional baggage comes with medical studies, especially when you’re not making any money,” Dr. Thomas said.
“The struggle is hard these days, not only for an internship but getting on to a training pathway. I think that really adds to students’ stresses and workloads because everyone’s trying to get that Ph.D. or do that extra research project to stand out from the growing crowd.”

John Bryant has turned his efforts to fundraising for Beyond Blue after his father and respected gastroenterologist Dr. Andrew Bryant took his own life.
Chloe’s relatives want to see safe working hours, breaks, more adequate compensation and a serious focus on cultural change.
“That work falls to other colleagues that are already under immense stress … you’re seen as that person who’s letting the team down,” her sister Micaela said.
WE NEED TO DO MORE
Since his father’s death, John has thrown himself into initiatives that raise funds for and awareness of mental health.
Last year, he and his brother Nick took part in the Noosa triathlon and together raised $28,000 for Beyond Blue.
John signed up again this year and has so far raised more than $8000 for the charity. He is also an ambassador for Bicycle Queensland, acting as a mental health ambassador.
“It has been completely devastating. This isn’t something we’ll ever really get over. You become better at dealing with it, I think, but it’s still very difficult. It doesn’t go away.
“I’m trying to make some positives out of a really bad experience. Hopefully, we can learn from what happened and help some other people.”

Doctors are unwilling to seek help if they’re struggling with mental health issues, research has found.
In her piece, Dr. McCormack said a raft of system-wide changes were needed, including senior doctors investing in the improvement of their physical and mental health to set an example for juniors.
“Doctors need to learn how to be kinder to themselves and extend compassion towards the struggles of both junior and senior colleagues,” she said.
“Medical students should be selected not just on academic performance, but increasingly sophisticated aptitude testing should be used.”
A greater monitoring of the mental health of medical students should be prioritized, she said, and broader wellbeing programs for professionals at all levels should be mandatory.
“Helping doctors build resilience may be protective against burnout and suicide in times of personal hardship,” she said.
If you or someone you know needs help, please contact Lifeline on 13 11 14 or visitlifeline.org.au.
Find out more about the work of Gotcha4Life by visiting gotcha4life.org.