By
#SeattleTimes #MentalHealthProject reporter
Three years ago, therapist Canh Tran suddenly found himself on the frustrated end of a long string of phone calls.
Tran knew very well that many of his clients had struggled to find a suitable #therapist. Now he was the one dialing the phone, seeking help for himself.
Straight to voicemail. Leave a message. Send an email. Maybe a text?
Repeat.
Repeat.
Repeat.
Tran, who lived in a refugee camp at age 2 before moving to the U.S. at age 3 — and #Washington state around age 8 — is the only living member of his immediate family. In a tragedy that rocked his life and the Catholic #Vietnamese community he was a part of, his #parents and three brothers died in the mid-2000s of carbon monoxide poisoning from a generator in the garage after a winter windstorm took out power at the family’s Burien home. Tran was away at college at the time.

The #MentalHealthProject is a #SeattleTimes initiative focused on covering #mental and #behavioralhealth issues. It is funded by Ballmer Group, a national organization focused on economic mobility for #children and families. The #SeattleTimes maintains editorial control over work produced by this team.
To work through subsequent symptoms of #anxiety and #depression, Tran wanted professional help. His work as a clinical social worker, he thought, afforded him more insight into the #mentalhealthcare system than most. But, as he soon found out, there are no shortcuts to accessing therapy.
He called his insurance company. “It doesn’t sound like your symptoms are that bad,” said the person on the other end, recalled Tran, who now practices in #Seattle. To get care, he first had to prove therapy was a medical necessity — a process that can include anything from getting a formal #mentalhealth diagnosis, to sharing personal or sensitive details about symptoms. If his insurance found him eligible, it would be up to him to find a clinician.
The gulf between the needs of those seeking therapy and the capacity of the #mentalhealth workforce to provide care is huge. In Washington and across the country, even those who are well-prepared to seek #mentalhealthcare — like Tran — can spend crucial months struggling with barriers related to #therapist availability and insurance before finding the right match.
Societal #stigma against #mentalillness has long undercut the way conditions are researched, funded and treated. Too few people are graduating from therapy training programs. In general, too few people are working as #mentalhealthproviders: Only 12% of Washingtonians live in a place where the public’s #mentalhealth needs can be met. And the workforce is predominantly white, creating unique roadblocks for #peopleofcolor.
#Mentalhealth resources for #BIPOC and #LGBTQ+ communities
- Where to find diverse #mentalhealthresources in #Seattle
- Canh Tran’s list of recommended resources
- Lambert House’s suggested resources for #LGBTQ+ youth
- #Mentalhealthresources in #KingCounty and #Washington state
Insurance companies’ policies and low reimbursement rates contribute to a cascade of other issues. Some bureaucratic tape is so thick it’s pushing providers to only accept clients who can pay out of pocket — an often insurmountable burden for lower income folks. Some providers say insurance reimbursement rates are so low they’re leaving the workforce altogether.
These concerns are increasingly coming out of the shadows. The refrain “why is it so hard to find a #therapist?” is a new fixture in #pandemic-era conversations. Families and friend groups are talking openly about their feelings of #loneliness, grief and loss. And more people are shedding the social #stigma that’s kept them from seeking care.
Actually getting a therapy appointment, though — that’s proving magnitudes more difficult than before, experts say.
“Pre-#pandemic, it was challenging to find a #therapist but … you would probably find someone with an opening somewhere,” said Samantha Slaughter, director of professional affairs for the #WashingtonState Psychological Association. “Now,” she said, “that feels almost impossible.”
Before the #pandemic, people may have made a handful of phone calls before finding an opening, Slaughter said. She estimates that number is now closer to 30 or 40. According to a #CDC survey from late September and early October, about 12% of Washingtonians reported needing counseling or therapy, but didn’t get it.
Access to #mentalhealthcare
The #SeattleTimes’ #MentalHealthProject has been exploring issues of access to #mentalhealthcare. A series of stories published in December took a deeper look at why it’s so hard to get help when you need it.
Why it’s so hard to find a #therapist, and stories from readers
Naomi Ishisaka: Finding care shouldn’t be this hard
Guide: What to know when looking for therapy
How Washington’s approach to #mentalhealth has changed
Mapping #mentalhealth: Washington’s capacity for care
Guide: Tips for when you can’t find a #therapist
Finding more intensive care, like scheduling an appointment with a #psychiatrist who can prescribe medication, is even more difficult. In general, more than 50% of #Washington #adults with a #mentalillness receive no treatment, a recent report from #MentalHealth #America suggests.
“To ask somebody to put forth that much more effort in finding a #therapist these days, when it’s hard enough to go to email or make that first phone call anyway, it’s asking a lot,” Slaughter said.
In acknowledgment of this, a small handful of states — not including #Washington — are passing laws requiring that insurance companies cut wait times for #mentalhealth appointments. In October, for instance, California’s governor signed a law requiring insurers to cut wait times for #mentalhealth appointments to no more than 10 business days; to comply, insurers may have to hire or contract with more therapists, a prospect that could force companies to make their policies or reimbursement rates more attractive to providers.
Slaughter and others say they’re eager to see how laws like this are enforced, especially given increasingly high demand. More than 80% of #psychologists who treat #anxietydisorders, and 72% who treat #depression, say requests for #mentalhealthcare are up since the start of the #pandemic, an October survey from the #AmericanPsychologicalAssociation suggests. More than 40% of #psychologists say they can’t meet their current demand.
For someone like Tran — who relied on insurance to pay for therapy, and who expected his provider to understand and respect his cultural background — the barriers to care were particularly steep. He contacted about 15 providers before finding three or four who seemed like a good fit.
#Mentalhealth resources for #youth
- #Seattle youth guide to multicultural #mentalhealthresources
- What you need to know about #mentalhealth and #schools
- #Mentalhealthresources in #KingCounty and #Washingtonstate
In his own practice, most of his clients — many of whom are #queer, #transgender and #peopleofcolor — find him through word of mouth and pay out of pocket on a sliding scale (Tran can’t yet accept insurance because he isn’t fully licensed. Provisionally licensed social workers need to work under supervision before they’re eligible to receive a license and work independently). But like many of his colleagues, Tran isn’t taking new clients.
On his website, a pop-up message appears: “Unfortunately, my practice is full.”
The right fit
Tran says he often refers callers to other providers he knows and trusts. He lists free resources on his website, including local and national #therapist directories devoted to specific gender identities and #racial groups.
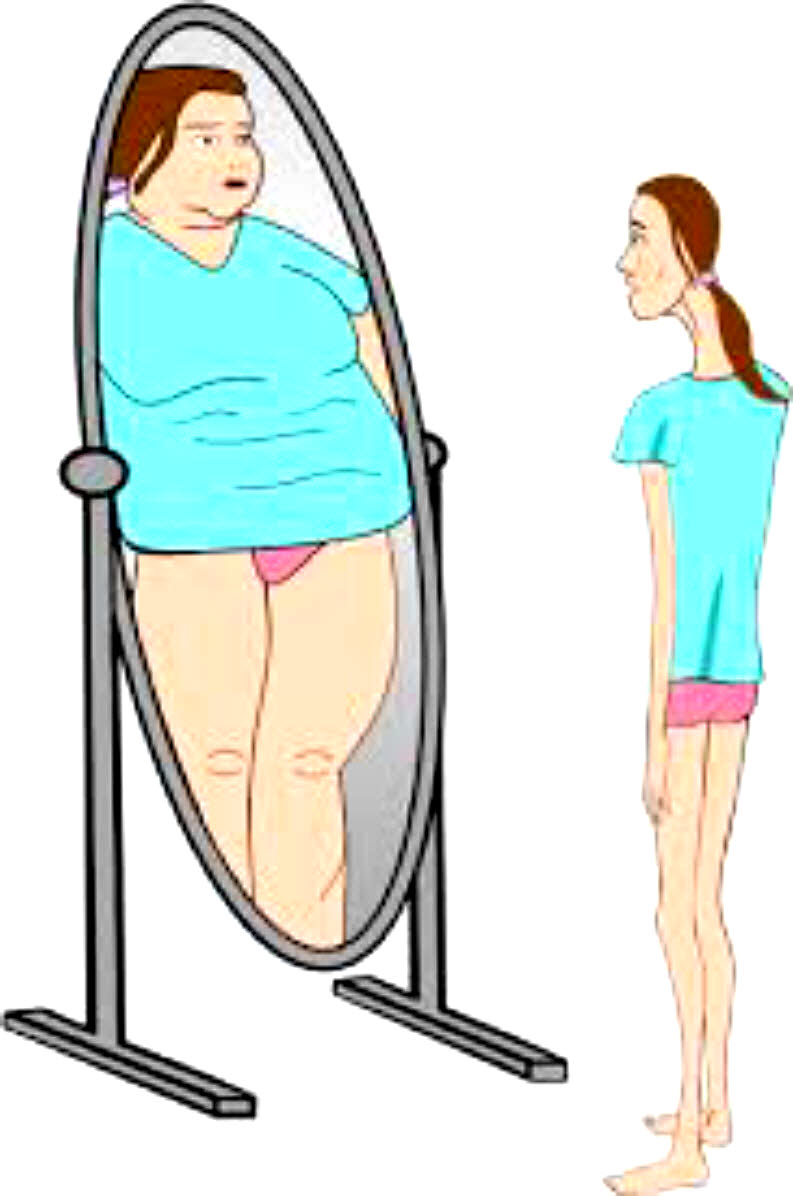
For people with marginalized identities, especially those who’ve experienced trauma, it’s easy to feel tokenized, misunderstood or unsafe in the presence of a #therapist who lacks specialized training or personal experience with #mentalhealth concerns, he said. More so than other areas of the medical world, finding the right “fit” between a #therapist and #patient is critical to whether the therapy is effective, he and other experts say.
“Research shows when you like, trust and vibe with your #therapist, it just works better,” he said.
The right “fit” includes a lengthy list of considerations, said Mollie Forrester, director of #patient and family experience in the department of psychiatry and #behavioral sciences at the #UniversityofWashington. Clients have to think about the type of therapy they’re interested in, their treatment goals, whether their schedule aligns with their therapist’s, and whether it’s important to them that their #therapist understands their religion, cultural background or gender identity. That’s on top of basic questions, like if the #therapist works with their insurance, Forrester said.
A lack of diversity in the #mentalhealth workforce means that some people struggle more than others to find good care. The #mentalhealth workforce is becoming more racially diverse, but it is still dominated by people who are white.
#Mentalhealth resources from The #SeattleTimes
- #Mentalhealthresources in #KingCounty and #Washingtonstate
- Where to find diverse #mentalhealthresources in #Seattle
- #Mentalhealthresources for those struggling with life amid a #pandemic
- Here are the basic facts about #mentalhealth and treatment in #Washingtonstate
Having a complex diagnosis, or several diagnoses, can also make it tricky to find care.
Five years ago, while living in Bellingham, Sarah Bond-Yancey called 40-some #therapists in Whatcom and Skagit counties who seemed like a good match.
“There were three key reasons why someone turned down working with me,” Bond-Yancey said. Reason one: They were full. Reason two: They didn’t accept Bond-Yancey’s insurance.
“The third thing I ran into, which was the most upsetting to me, was #therapists being uncomfortable with my diagnoses.”
Bond-Yancey has dissociative identity disorder, #bipolardisorder, obsessive compulsive disorder and attention-deficit hyperactivity disorder. #Therapists told Bond-Yancey they weren’t knowledgeable enough or didn’t feel comfortable treating someone with this combination of conditions. The dissociative identity disorder diagnosis makes finding care particularly hard, says Bond-Yancey, adding that having 23 different self-states means their “entire identity shifts randomly and constantly and abruptly” (Bond-Yancey uses they/them pronouns).
Of the therapists Bond-Yancey reached out to, several never responded. Then, Bond-Yancey’s insurance changed. A peer support group was one of the few services available. It took more than a year to find a therapist with an opening.
After a move to Olympia in 2019, the process started all over again.
“All in all, I think I’m approaching 100 #therapist contacts over the past four to five years, with no results,” Bond-Yancey said.
Red tape
Iris Smaus, 74, was coming to terms with certain regrets, and wanted help moving on. Finding a #female #therapist in her age group, which was important to her, shouldn’t have been impossible. About 65% of #psychologists are #women and the average age among the #psychologist workforce is 49 years.
Plus, Smaus has Medicare and commercial insurance. But she still struggled to find someone in-network for about five years. Smaus, who lives in north Kitsap County, said one of the few people she could find who took her insurance was a male therapist in Suquamish. Access to #mentalhealthcare in Washington’s rural corners is particularly difficult, state data suggests.
When she couldn’t find anyone else, she started calling #therapists in Edmonds and Seattle — both a ferry ride away. “I just didn’t have much luck,” she said, until she eventually found a clinical social worker this year.
“For people that are really desperate to find somebody, it must be awfully daunting,” Smaus said. “It was for me.”
More than a decade ago, federal lawmakers passed the #MentalHealth Parity and Addiction Equity Act, which requires that if insurance companies provide coverage for #mentalillness and substance use disorders, those benefits must be equal to benefits provided for physical health conditions.
But in reality, parity doesn’t mean access — insurers can choose to exclude #mentalhealthcare from coverage plans. And having insurance with mental health care coverage far from guarantees a therapy appointment. Since the law passed in 2008, insurance companies have found sophisticated ways to limit #mentalhealthcare, experts say.
Tran, Bond-Yancey and Smaus all turned to lists of names offered by their insurance providers. But such lists are often outdated. Insurance companies’ so-called “ghost networks” sometimes include #therapists who have moved, stopped taking insurance — even died, Tran said. Ghost networks are frustrating for clients, and make insurers appear to work with many more providers than they do.
#JamesDonaldson notes:
Welcome to the “next chapter” of my life… being a voice and an advocate for #mentalhealthawarenessandsuicideprevention, especially pertaining to our younger generation of students and student-athletes.
Getting men to speak up and reach out for help and assistance is one of my passions. Us men need to not suffer in silence or drown our sorrows in alcohol, hang out at bars and strip joints, or get involved with drug use.
Having gone through a recent bout of #depression and #suicidalthoughts myself, I realize now, that I can make a huge difference in the lives of so many by sharing my story, and by sharing various resources I come across as I work in this space. #http://bit.ly/JamesMentalHealthArticle
We’d like to hear from you.
The #MentalHealthProject team is listening. We’d like to know what questions you have about #mentalhealth and which stories you’d suggest we cover.
Get in touch with us at mentalhealth@seattletimes.com.
Dr. Susanne Quistgaard, medical director at Premera, said many insurance companies struggle to keep provider directories up to date. Even when the company asks providers for updated information, they don’t always respond. A new federal law may help eliminate some of the outdated information: On Jan. 1, the federal “No Surprises Act” takes effect, forbidding #patients from receiving surprise medical bills and requiring that insurers update provider directories every 90 days.
Insurance companies’ accreditation is dependent on having an adequate network of providers; to meet increasing demand, for example, a spokesperson for #KaiserPermanente said the company is in the process of hiring more #behavioralhealth staff, and a spokesperson for Regence said the company is expanding its network of #therapists.
Premera recently tried to expand its network, Quistgaard said, by reaching out to its most frequently used out-of-network providers. “It wasn’t very successful, I have to say,” she said. But Quistgaard didn’t offer specifics when asked about why providers declined invitations to join the company’s network.
More than a half-dozen #therapists interviewed for this article said most insurance companies don’t reimburse them enough to justify the paperwork involved. Asking clients to pay out-of-pocket is logistically much easier, they said.
For example, some insurance companies require therapists to regularly submit records showing a patient’s therapy is medically necessary; one #therapist reported having to write 5-6 page reports every six months about individual #patients to prove the care was necessary.
Other companies threaten to audit therapists who are perceived as billing too many hourlong therapy sessions, Slaughter said, instead of 45-minute sessions, which are generally reimbursed at a lower rate. A recent letter from Regence, for example, said the company was reviewing a therapist’s billing practices but that the letter was “not intended to question a provider’s treatment methods or clinical judgment.” It went on to say, however, that if the #therapist continued to bill for a higher than usual number of hourlong sessions, the company may contact them for “further validation and education.”
A spokesperson for Regence said the letter was sent to 2.5% of its contracted #behavioralhealthproviders and was “meant to be informative and respectful.” But some #therapists perceive letters like this as threatening, Slaughter said.
Premera and other companies, including #KaiserPermanente and Regence, declined to share their reimbursement rates, citing contract confidentiality clauses. But they said their rates are competitive.
According to Slaughter, commercial insurance plans tend to reimburse $80-$140/hour for an hourlong appointment depending on whether they’re a #psychologist or master’s-level #therapist. Those rates might sound high, Slaughter said. But many #therapists only bill 25-30 hours each week, with the rest of their time consumed by writing chart notes, calling #patients or scheduling sessions.
For someone who bills 25 therapy hours a week, half of their $100 hourly income is quickly eaten up by taxes, business expenses and rent, Slaughter said. Individual #therapists can try to negotiate higher pay, but confidentiality agreements — a condition of working with insurance companies — and antitrust laws bar individual #therapists from sharing their rates with peers or attempting to negotiate as a group, she said.
Jane Palmer, who specializes in trauma and has worked as a psychotherapist in #KingCounty for 25 years, said she spends about 24 hours with #patients each week, and four to six hours dealing with billing and other administrative tasks.
She’s only allowed to bill for the minutes she’s in a session with a #patient. One insurance company she used to accept cut her hourly pay by 25% about seven or eight years ago, she said. At another company, her reimbursed hourly rate has ticked up by less than $4 over the past decade. Some younger #therapists she knows have left the field because their rates are so low and they are their family’s primary earner.
“I find this work amazingly satisfying because people actually do get better,” she said. But, she added “The economics of psychotherapy don’t make any sense. Nobody would ever be a #therapist if they were interested in making money.”
Hannah Furfaro: hfurfaro@seattletimes.com; on Twitter: @HannahFurfaro. Hannah Furfaro is a #mentalhealth reporter at The #SeattleTimes. She has a master’s degree in science and health journalism from Columbia University, and wrote about neuroscience and psychiatry before joining The Times. She previously published stories in Science, The Wall Street Journal and The Atlantic, among other places. Send her tips at hfurfaro@seattletimes.com or find her on Twitter @hannahfurfaro.