Share on FacebookShare on Twitter

BY REBECCA RUIZ
#JamesDonaldsononMentalHealth –
Welcome to the “next chapter” of my life… being a voice and an advocate for #mentalhealthawarenessandsuicideprevention, especially pertaining to our younger generation of students and student-athletes.
Getting men to speak up and reach out for help and assistance is one of my passions. Us men need to not suffer in silence or drown our sorrows in alcohol, hang out at bars and strip joints, or get involved with drug use.
Having gone through a recent bout of #depression and #suicidalthoughts myself, I realize now, that I can make a huge difference in the lives of so many by sharing my story, and by sharing various resources I come across as I work in this space. #http://bit.ly/JamesMentalHealthArticle
In February 2015, Lily Allen intended to take her own life. A freshman in high school at the time, she might’ve succeeded had she not confessed that plan to a concerned friend, who then called the police. Officers showed up at her parents’ home in Frisco, Texas, and Allen soon checked into the psychiatric unit at Children’s Health, in Dallas, for a week.
Allen had seen a therapist in elementary and middle school to talk through friendships gone sour. She’d been bullied on more than one occasion and experienced #anxiety. Allen felt overwhelmed by the long struggle to belong.
When it comes to depictions of #suicide in media and pop culture, there is a dangerous perception that someone like Allen, who is inclined to take her own life, cannot be stopped. For #teens, in particular, that myth may be hard to shake; suffering can seem never-ending from the vantage point of adolescence.
But that myth may have been reinforced in recent years thanks to the portrayal of #teen #suicide on the Netflix show 13 Reasons Why as well as news reports on the rising rate of suicide, including a noticeable spike among 10- to 14-year-olds.
Allen, 18, speaks openly about her experience to offer hope in contrast to bleak stories about teen suicide. Now a freshman at a performing arts college, Allen is pursuing her dream to become a professional dancer. She says that finding the right treatment — an intensive, skills-based out-patient program at Children’s Health — ultimately stopped her #suicidalthoughts and behavior.
“It’s been a few years,” she says, referring to her #suicidal feelings. “It was just about really working hard in therapy and the [out-patient program], putting my best foot forward, and knowing things I can control and knowing things I cannot control, identifying things that I can control and making them part of the situation that makes me happy.”
Allen’s experience inspires optimism that should be more widespread, because we know more than it seems about how to prevent #teen #suicide. It doesn’t always require a hospital-based program like the one Allen attended.
We know more than it seems about how to prevent #teen #suicide.
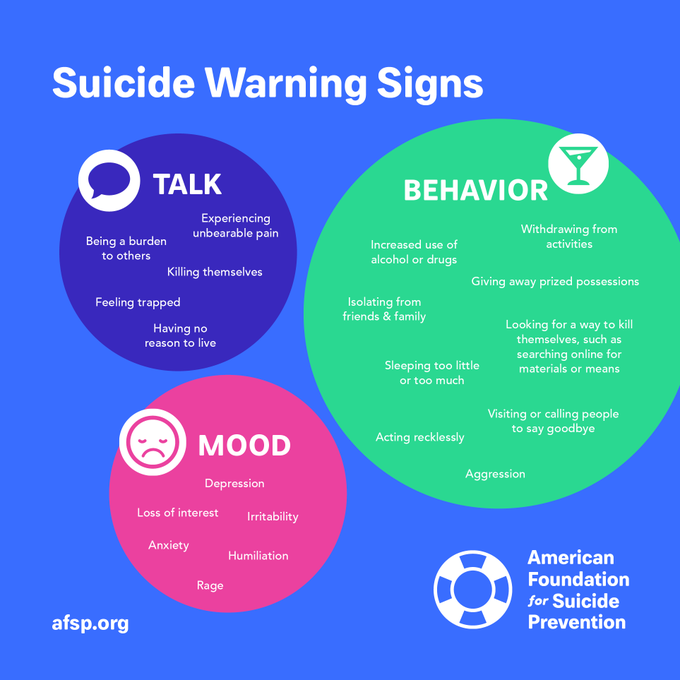
Common sense approaches effective for preventing #suicide in general — like talking about #mentalhealth and asking specifically about #suicide, making a safety plan, restricting lethal means, identifying “gatekeepers” trained to spot #suicide risk factors and warning signs and provide resources, and knowing what to look for in a treatment — can also help save #teens’ lives. Meanwhile, promising interventions currently being studied suggest we’ll have more precise ways to prevent #teensuicide in the coming years.
Here are practical steps anyone can take to help stop a #teen from taking their own life:
1. Talk about #mentalhealth and #suicide
Research shows parents often aren’t aware their adolescent child is thinking of dying, and that teens deny experiencing #suicidalthoughts. More than two-thirds of #suicidal adolescents don’t see a #mentalhealthprovider either, likely because their caregivers don’t realize they’re struggling, according to a survey of more than 10,000 adolescents. This complex dynamic is partly why it feels challenging to detect #suicidrisk among teens, and it’s why #suicideprevention experts urge adults learn the warning signs and start conversations about #mentalhealth with the young people in their lives.
Some worry that raising the subject unprompted will put the idea of #suicide into a #teen’s mind, but research suggests that isn’t the case. In fact, acknowledging and talking about #suicide may actually reduce those feelings.
Acknowledging and talking about #suicide may actually reduce those feelings.
Lisa Horowitz, a staff scientist and pediatric psychologist at the #NationalInstitutesofHealth who works on suicide prevention, says conversations about #mentalhealth between caregivers and children can start at an early age, with an emphasis on developing lifelong coping skills for dealing with stress and emotional highs and lows. Horowitz recommends talking about how the brain can create cognitive distortions, or “faulty” thinking patterns, that can disproportionately focus our attention on negative emotions or beliefs, including #suicidalthoughts.
Teens benefit from knowing that cognitive distortions are a common phenomenon anyone can experience, and that they can make someone feel helpless — a warning sign that they need help. Horowitz says coping skills like talking to a trusted adult, calling a crisis or #suicidehotline, connecting with a good friend, or taking a walk can help quiet or reduce intrusive thoughts.
The trick for any caring adult having this conversation with a #teen is to model the behavior themselves, says Horowitz. That means not only being emotionally honest with a child but also consistently demonstrating what it looks like to use different coping skills in response to #stress, #anxiety, disappointment, and other difficult experiences.
Research also indicates that treating parents for their own #depression may positively affect their child’s #mentalhealth, which is why Horowitz recommends that families consider prevention a collective effort.
2. Make a safety plan
When a teen indicates they’re #suicidal, it’s critical to help them make a safety plan. That document can be a list of warning signs that crisis might be imminent; coping skills to manage those emotions; people and places that can provide positive distractions; trusted loved ones and professionals to contact; and ways to make an environment safe from potential self-harm.
Do you know the suicide warning signs?
A study published last year found that #suicidal adults who visited the emergency department and received assistance creating a safety plan, along with follow-up contact from a provider via telephone, nearly halved their odds of #suicidal behavior over six months compared to those who didn’t receive the same intervention. While the study wasn’t specific to adolescents or teens, prevention experts believe younger #suicidal patients also benefit from safety planning.
3. Restrict access to means of #suicide
It might seem obvious to keep a suicidal teen away from items that could enable self-harm, but it’s not a message young people and their caregivers consistently hear from clinicians and medical professionals. Nor do they necessarily think, on their own, to comb through cabinets and remove medication, firearms, sharp objects, or other implements that could be used in a #suicide attempt. Research, however, has shown that reducing lethal means is associated with decreases in the #suicide rate. One small study published in 2016 found that when parents of #suicidal children received counseling on restricting lethal means, they were later more likely to have locked away medicine and firearms.
4. Identify “gatekeepers” trained to spot signs of #suiciderisk and provide resources
The “gatekeeper” model relies on training community members, particularly adults, how to recognize that youth may be at risk for #suicide. Such training can happen at schools, community health centers, and other settings where staff frequently come into contact with youth. The trained gatekeepers are prepared to identify risk in vulnerable youth and connect them with #mentalhealthandsuicideprevention resources when necessary. Research suggests that gatekeeper training is associated with reductions in youth #suicide deaths and attempts.
Cheryl King, a professor of psychiatry and psychology at the University of Michigan who studies #suicideprevention, believes the approach can have positive benefits because adults in regular contact with youth may be best positioned to recognize #suiciderisk, and because it uses human connection to bring an individual’s risk out into the open, which is followed by a caring effort to get a #teen the resources they need.
We need to come together to normalize talking about #mentalhealth. It needs to be something everyone is comfortable talking about.
“A [gatekeeper] can say, ‘I’m concerned, I care about you and what’s going on … I would like to try to take a next step with you, to get some help,'” says King.
Though gatekeeper training isn’t yet widespread, King says there are communities that have received funding to implement it, or where “champions” of the approach brought training to schools and other relevant settings. More than 100 middle and high schools in central and southeastern Ohio, for example, introduced a gatekeeper program called SOS Signs of Suicide in partnership with Nationwide Children’s Hospital, in Columbus. The program has shown encouraging results in reducing #suicidalthoughts and behaviors and improving students’ knowledge about #mentalhealth.
5. Know what to look for in treatment
If a teen seeks or needs formal treatment for #suicidal thinking and behavior it’s important to know as much as possible about the available options. Some therapists may have little experience working with #suicidal teens, but could be skilled at treating #depression and #anxiety. Other providers may specialize in reducing #suicidal thoughts and behavior, with a track record to match.
In general, we know that skills-based techniques like cognitive behavioral therapy and dialectical behavioral therapy, as well as medication, are among the effective ways to treat #suicidal adults, though much less is known about how teens respond to those treatments. A randomized, clinical trial that used DBT to treat #suicidal adolescents found that it reduced repeat #suicide attempts and self-harm. Yet it’s unlikely that teens or their caregivers know the difference between treatments, which is why they should ask whether a certain approach or technique is based on evidence and research.
Randy Auerbach, a clinical psychologist and associate professor at Columbia University who works with and studies #suicidal teens, says their emotions can fluctuate rapidly. They may spend an hour in their therapist’s office feeling safe, enhancing or refining their coping skills, and then leave that space only to experience a breakup, rejection, or psychological distress.
If you or someone you know feels hopeless or like they have no reason to live, call 1-800-273-TALK (8255) for help and support.
Auerbach likens this dynamic to teaching a #teen how to hit a curve ball. As much as a #teen can be coached on how to perfect their swing, when a curve ball comes at them in real life, they might feel incapable of hitting it. When they’re feeling heightened emotional distress, #teens may be less inclined to use their coping skills, and in some cases, make regrettable choices.
Auerbach says that part of the problem is providing seamless access to care for teens, particularly those at high risk for #suicide. Reducing youth #suicide may mean removing barriers teens and their caregivers encounter when trying to access effective treatment.
Looking forward
When Lily Allen enrolled in the outpatient program at Children’s Health in Dallas, she found the emphasis on group, individual, and multi-family therapy, in combination with DBT, cognitive behavioral therapy, and learning coping skills, dramatically improved her ability to handle #suicidal thoughts and feelings.
Allen says that the program, known as #SuicidePrevention and Resilience in Children (SPARC), is where she first learned about coping skills, including a technique for evaluating her thoughts for unhelpful thinking patterns. She began looking at her emotions like she might a flowchart, noting her own vulnerabilities, what might’ve happened to prompt negative feelings, the thoughts that accompanied those feelings, and what positive things she could focus on instead.
But she also just learned to embrace enjoyable activities as a means of coping. Coloring, puzzles, and journaling, all things she’d previously loved but stopped doing, once again became mainstays of how she spent time. Allen says she realized that screen time and social media had distracted her from simple pleasures.
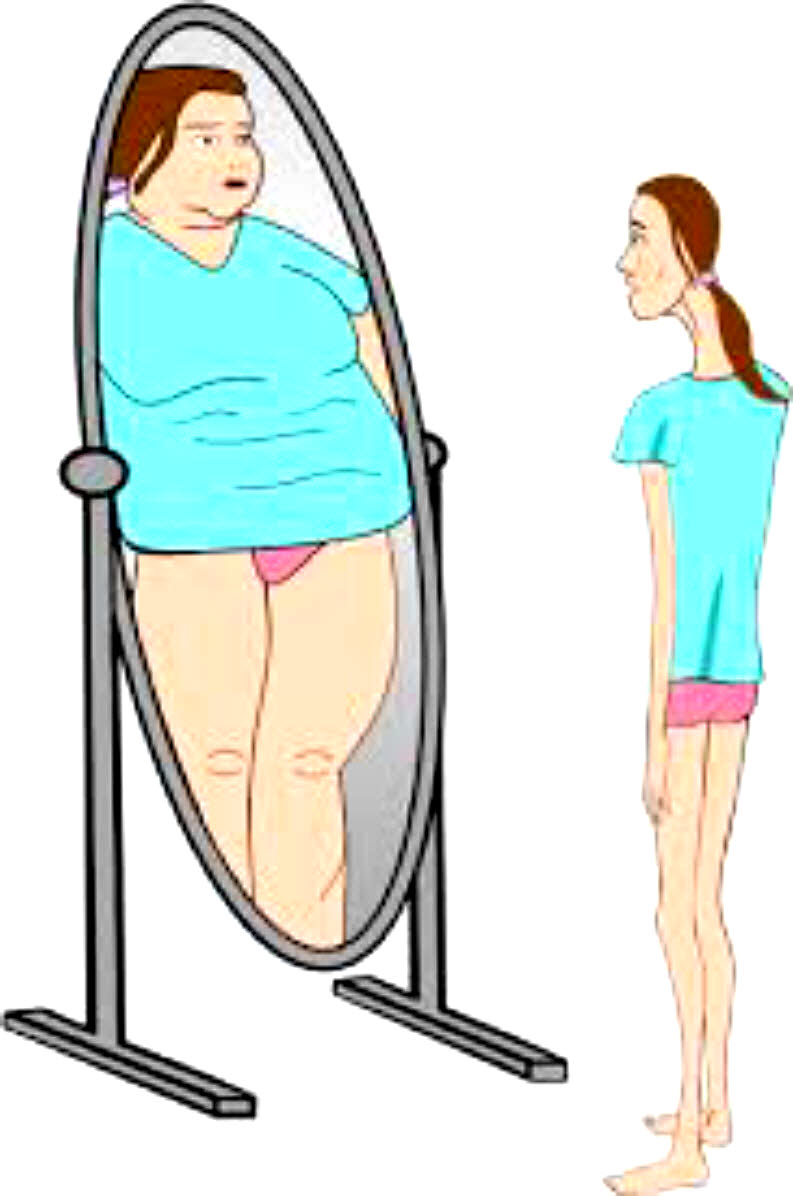
“I was so focused on looking a certain way, acting a certain way … I was a whole different person because of the way I wanted to be perceived on social media,” she says.
Allen spent about a month in SPARC and then transitioned to seeing a therapist recommended by the program. She says that maintaining her recovery, along with the new skills she’d learned, took hard work at first and then eventually felt like a natural instinct. (Allen’s gratitude for her experience has extended to fundraising for Children’s Health; she’s raised thousands of dollars to benefit SPARC through dance performances in the past few years.) A study of SPARC’s outcomes found that patients were overwhelmingly satisfied with the program and that it improved #depression and #suicidal thinking and behavior.
The results need to be replicated with a control group in order to consider SPARC an effective treatment for the broader population, but the program’s preliminary success points to a future in which teens can access numerous #suicideprevention programs.
That could include options like gathering information from teens’ smartphones (with their consent) in order to develop algorithms that predict when they might become #suicidal, a study currently being co-led by Auerbach and his fellow collaborators. King, at the University of Michigan, is hoping to replicate the results of her study of an intervention designed to let #suicidal adolescents nominate “caring adults” who are trained to support them following hospitalization.
Jeff Bridge, an epidemiologist and director of the #CenterforSuicidePrevention and Research at the Abigail Wexner Research Institute Nationwide Children’s Hospital in Columbus, is working with other researchers to adapt an effective #suicideprevention program for adults known as Collaborative Assessment and Management of Suicidality (CAMS) for 5- to 11-year-olds. (One of the collaborators is David Jobes, the researcher who developed CAMS). Another team of researchers is creating an adaption of CAMS for #teenagers.
“I’m not really scared to share how I feel anymore.”
It may be years before we can declare any of these and other emerging interventions as definitively effective, but researchers are hopeful that we’ll get better at preventing #teen #suicide, even if the news now is often discouraging.
The relatively slow progress is also a reminder that no single program, treatment, or intervention will stop #teen #suicide. Instead, it takes varied approaches that reach #teens in different ways — and adults who can help lead them to safety.
Allen knows first-hand what that means and how it can change a teen’s life.
“I’m not really scared to share how I feel anymore,” she says.
If you want to talk to someone or are experiencing #suicidal thoughts, text the Crisis Text Line at 741-741 or call the #NationalSuicidePreventionLifeline at 1-800-273-8255. Here is a list of international resources.