By Marya J. Cohen
One Monday about a year ago, I walked down the hall of our clinic to ask my colleague’s advice about a #patient. I often sought his guidance over the years.
A grandfatherly figure, Elisha Atkins — we called him “Skip” — loved examining puzzling rashes, talking to #patients in their native language (he spoke several) and thinking out loud through a complex medical decision. Skip would always ask for follow-up weeks later. His #patients loved that he remembered the names of their family members, and when we would go out to eat in the neighborhood, I was usually late for my afternoon #patients because he stopped to say hi to everyone we passed.
That Monday when I asked Skip’s opinion — this time, on a troubling case of weight loss — I knew I would find him with his tie askew and his glasses crooked, which I did. He sat in his chair and listened, asking questions about food insecurity and other social determinants of health.
But that Monday was different. After we talked, Skip canceled his #patients for the week, left the office and killed himself.
We were all blindsided. How did we not know? Was he depressed? Was he reaching out for help? If this could happen to him, who else could it happen to?
We would later learn about his struggles with other #healthissues, including possible #dementia, but confusion still reverberated in our exam rooms and meetings. Administrators from the hospital met with us and talked of “making time for wellness” and “taking care,” but it rang hollow, and grief was soon swallowed up by the coming tide of the #coronavirus #pandemic.
I think of Skip often these days, as our community of Chelsea is one of the epicenters of the novel #coronavirus in Massachusetts. He dedicated his 40-year career to the MGH Chelsea HeathCare Center caring for refugees and immigrants. I am certain he would have been the first to volunteer to see #covid-19 #patients in our respiratory illness clinic, or he would have been handing out food supplies. Perhaps seeing the worsening disparities in our community would have further depressed him.
#JamesDonaldson notes:
Welcome to the “next chapter” of my life… being a voice and an advocate for #mentalhealthawarenessandsuicideprevention, especially pertaining to our younger generation of students and student-athletes.
Getting men to speak up and reach out for help and assistance is one of my passions. Us men need to not suffer in silence or drown our sorrows in alcohol, hang out at bars and strip joints, or get involved with drug use.
Having gone through a recent bout of #depression and #suicidalthoughts myself, I realize now, that I can make a huge difference in the lives of so many by sharing my story, and by sharing various resources I come across as I work in this space. #http://bit.ly/JamesMentalHealthArticle
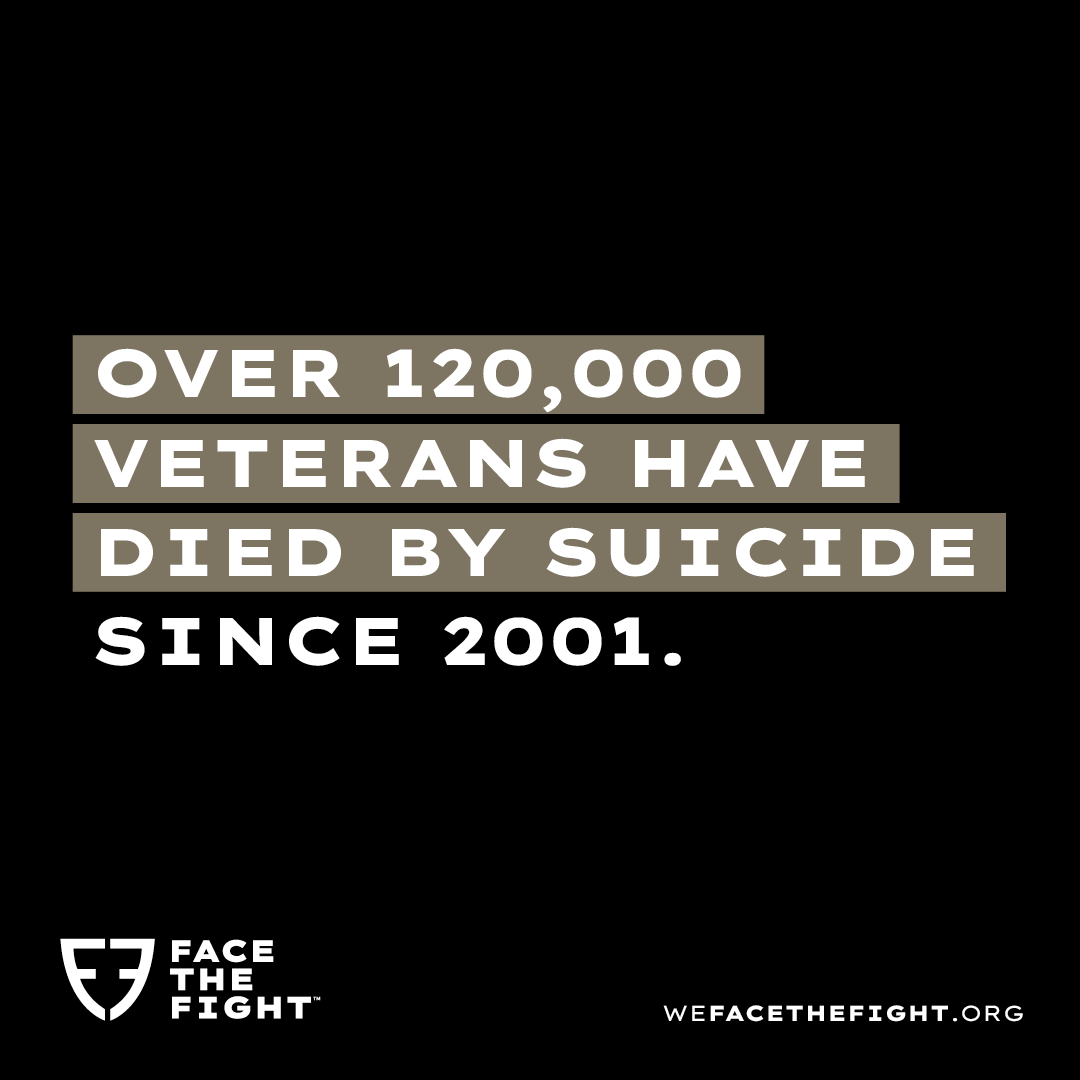
Although #suicide across the world is declining in some areas, this is not true in our country. #Suicide rates in the #UnitedStates are increasing, and now account for about 1.5 percent of deaths annually since 2000. #Physicians, in turn, have the highest rates of #suicide of any profession, with roughly one #doctor dying every day. That is nearly double the rate of the general population.
Self-care has been increasingly difficult for #patients and #physicians alike during these unprecedented times. Some experts note a potential “perfect storm” of growing #isolation, economic stress and decreased access to community support leading to a potential jump in #suicide rates during the #pandemic. For #healthprofessionals in particular, this warrants particular attention.
#Physicians who die of #suicide often suffer from undertreated or underdiagnosed #depression, a risk factor for #suicide itself. Often, due to #stigma, time constraints or confidentiality fears, #doctors are reluctant to seek help for #depression.
Last spring, I found myself poring over the story of #Lorna Breen, an emergency room #physician who killed herself in New York after treating countless #patients with the #coronavirus. I related to the overwhelming duty and guilt described in her obituary. Breen kept saying, “I couldn’t do anything.”
I’ve never been suicidal, but I felt despair in April. I remember coming home from hours on duty at the overwhelmed #covid-19 clinic and I felt overwhelmed myself. I couldn’t really describe what I was feeling — we’ve failed to normalize talking about #mentalhealth. Breen’s family established a fund for #mentalhealthcare in the wake of her #suicide, noting the difficulty she had seeking #mentalhealthcare in a system that often failed to acknowledge the deep burden of its providers.
At our hospital, a lot of time and money is spent on wellness efforts, and #physicians are surveyed annually about burnout. I can apply for grants for wellness, get coached on my career and (pre-#pandemic) take yoga classes. In March, our clinic was thinking about launching a #suicideprevention initiative called RU okay — and then #covid-19 happened.
What these workplace initiatives — which are not specific to health care — have in common is that they create space for talking about how hard things can be beyond passing exchanges in the hallway. Participants essentially pledge to check in on one another. A program out of Rutgers called Check You, Check Two encourages people each day to take time to ask themselves how they’re doing, and to talk to two co-workers to ask how they’re doing, as well. It is something I now strive to do as part of my practice.
While I support all endeavors to talk about #mentalhealthissues and decrease feelings of #isolation, we need to do more for #healthcareprofessionals. We need to create a dedicated center for the additional study of #physician #suicide. We lack data behind the prevention, incidence and risk factors of #physician #suicide.
We need to implement universal training in the prevention of #suicide, particularly during these times of #mentalhealth extremes.
There’s #loneliness and #isolation in many professions, but there’s something specific to what’s going on in #healthcare that doubles #suicide risk. The historical culture of medicine contributes to this: massive amounts of self-reliance and lack of attention to emotional well-being. We need to dispense with the pervasive notion that to be a “good #doctor” means to always be available — to always go the extra mile in advocacy (fighting for insurance coverage of that CT scan), availability (squeezing in another #patient) and accessibility (logging into electronic medical records at night to fill prescriptions).
Good #doctors always say “yes” to helping #patients in an effort to provide high-quality care. But when that comes at the expense of the #doctors’ own health, it’s not sustainable. The cost can be too high for some.
#Healthcareworkers have been lauded as heroes during the #pandemic, but all the clapping in the world doesn’t eliminate #isolation and #depression if one can’t hear it.
#Physicians need to work in teams, share responsibilities and build in time to talk about high-risk #patients and tough cases. We need to find regular ways to connect that aren’t one-off wellness activities. We need to establish boundaries around #doctors’ work and home time so both #patient and #doctor needs are met.
I think about one of the last emails my mentor sent before he died. It was uncharacteristic, because it revealed a deep sadness. He was a beautiful writer, and the email was about how siloed we are in medicine, all doing our own things, all our own islands. He called on us to collaborate more, to share our work more. He recalled talking with colleagues and how healing it was, and he commented that he was “spending far too much time alone at a computer doing documentation and email.” He said collegial energy “was better than espresso.”
I remember reading this and feeling a melancholy pang of recognition that stopped me in my tracks: Yes, there is burnout, but the real difficulty is that we’re not connecting with each other. We’re just going through the churn. Recently, we got funding to give some talks in his honor — it’s a start.
Our practice hasn’t been the same since he died. A year later, his #patients — now my #patients — still mourn his loss. We left the sign he had on his old office door — now a space for triage #nurses — that ubiquitous “Keep Calm and Carry On” sign. That’s the wish, isn’t it? Yet at some point this mantra lost its power. Maybe it should have read, “Are you okay?”
Marya J. Cohen, MD MPH, is a primary care #physician at MGH Chelsea HeathCare Center, medical director of the Crimson Care Collaborative, and a public voices fellow with the OpEd Project.

James Donaldson is a Washington State University graduate (’79). After an outstanding basketball career with WSU, he went on to play professional basketball in the NBA with the Seattle Supersonics, San Diego/L.A. Clippers, Dallas Mavericks, New York Knicks, and Utah Jazz. He also played for several teams in the European Leagues in Spain, Italy, and Greece, and he toured with The Harlem Globetrotters to wrap up his career. James was an NBA All-Star in 1988 while playing center for the Dallas Mavericks. In 2006, James was inducted into the Pac-10 Sports Hall of Fame and also the Washington State University Athletic Hall of Fame. In 2010, James was elected as a board member for the NBA Retired Players Association.
James frequently conducts speaking engagements (motivational, inspirational, educational) for organizations, schools, and youth groups.
In 2010, James was the recipient of the NBA Legends of Basketball ABC Award, awarded for outstanding contributions in Athletics–Business–Community.
He believes in being a role model for success and professionalism to the scores of young people to whom he devotes so much of his time. He currently serves on several boards and committees and is a member of many organizations.
James believes in developing relationships that create a “Win-Win” environment for everyone involved, and in being the best he can be!
For more information about James Donaldson or to request he speak at your event, contact him at:
www.StandingAboveTheCrowd.com
JamesD@StandingAboveTheCrowd.com
1-800-745-3161 (voicemail & fax)
James Donaldson is the author of “Standing Above The Crowd” and “Celebrating Your Gift of Life” and founder of the Your Gift of Life Foundation which focuses on mental health awareness and suicide prevention, especially pertaining to our school aged children and men.
If you’re interested in having James come and speak to your group of young adults, business entrepreneurs, aspiring political and community leaders, and athletic teams, please contact him at jamesd@yourgiftoflife.org and or leave a personal message for him at 1-800-745-3161. Keep up with him and read about how he is reaching out and making a difference in the lives of so many around the world at www.yourgiftoflife.org